There are some obvious signs of a poor night’s sleep — fatigue, irritability and trouble focusing, to name a few — but it can also have some hidden effects.
In a new study led by University of California, San Francisco (UCSF), poor sleep was linked to faster brain aging in middle-aged adults.
While previous studies have focused on older adults, the average age of the 589 people in this study was 40 years old, according to a press release.
‘SLEEP DIVORCE’ ON VACATION: TRAVEL TREND HAS COUPLES ‘BREAKING UP’ AT BEDTIME
The participants completed two sleep questionnaires five years apart. After 15 years, they underwent brain scans.
In a new study led by University of California, San Francisco, poor sleep was linked to faster brain aging in middle-aged adults. (iStock)
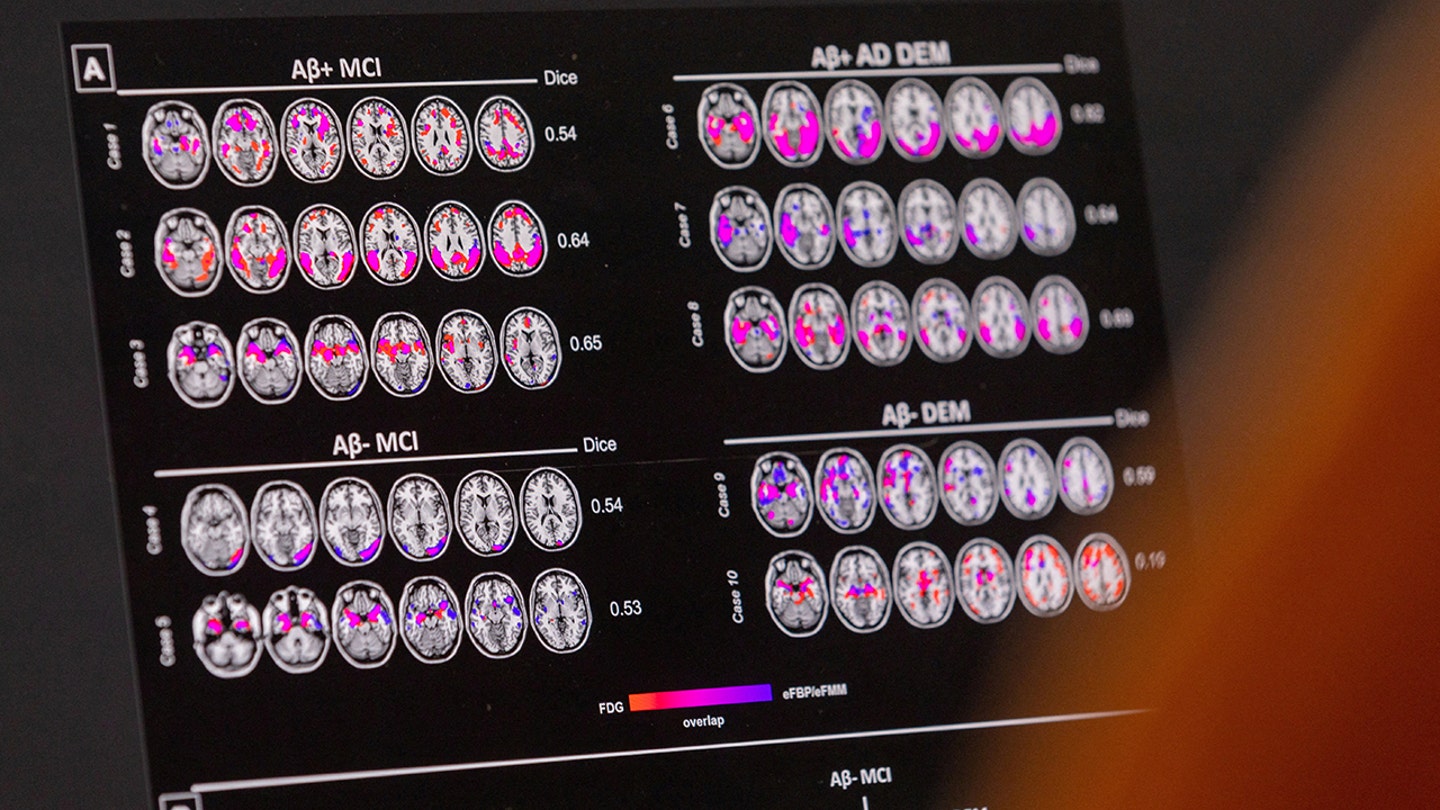
“We calculated brain age using a machine learning approach, using MRI data to estimate the amount of brain shrinkage corresponding to a specific age,” study author Clémence Cavaillès, PhD, a researcher at UCSF, told Fox News Digital.
“We showed that poor sleep that persisted over five years — and specifically when it related to insomnia symptoms — was found to be highly relevant to brain aging.”
‘WHY DO I HAVE RESTLESS LEGS AT NIGHT?’: ASK A DOCTOR
When evaluating sleep quality, the researchers looked at six poor sleep characteristics: short sleep duration, bad sleep quality, difficulty falling asleep, difficulty staying asleep, early morning awakening and daytime sleepiness.

“We showed that poor sleep that persisted over five years — and specifically when it related to insomnia symptoms — was found to be highly relevant to brain aging,” said the lead study author. (iStock)
Middle-aged participants with two to three poor sleep characteristics had a brain age that was 1.6 years older than those with no more than one poor sleep characteristic, according to Cavaillès.
Those with more than three poor sleep characteristics exhibited a brain age of 2.6 years older.
“Poor sleep that persisted over five years — and specifically when it related to insomnia symptoms — was found to be highly relevant to brain aging.”
The findings were published in Neurology, the medical journal of the American Academy of Neurology.
These findings are critical because they demonstrate that the link between sleep disturbances and brain health extends beyond older adulthood, suggesting that poor sleep in early midlife may already contribute to accelerated brain aging,” he said.

“If someone is facing persistent problems with sleep quality or insomnia symptoms, they should undergo further evaluation,” a doctor advised. (iStock)
Advanced brain aging is associated with cognitive decline and Alzheimer’s disease-related patterns, the researcher noted.
“Therefore, poor sleep may be an important target for early interventions aimed at preventing neurocognitive decline, even before the lesion’s accumulation begins.”
‘FOR BETTER SLEEP, HOW CAN I REDUCE NIGHTTIME BATHROOM TRIPS?’: ASK A DOCTOR
The researchers were surprised to find that there was not an association between sleep duration and accelerated brain aging, Cavaillès noted.
“Sleep duration in midlife may be influenced by numerous factors, such as work, stress, multitasking or menopause,” he told Fox News Digital.

Advanced brain aging is associated with cognitive decline and Alzheimer’s disease-related patterns. (iStock)
“Thus, it is also possible that its association with cognition is more complex during this critical period, and potentially more difficult to capture and/or less impactful.”
Overall, the study results suggest that the importance of sleep for brain health in midlife would be more closely tied to quality rather than quantity in midlife, the researcher added.
‘Integral relationship’
Dr. Jocelyn Y. Cheng, a New Jersey neurologist and spokesperson for the American Academy of Sleep Medicine, was not involved in the study but weighed in on the findings.
“This study provides further support for the integral relationship between sleep and brain health,” she told Fox News Digital.
‘HOW MUCH SLEEP IS TOO MUCH?’: ASK A DOCTOR
“The findings highlight particular aspects of poor sleep — specifically early morning awakening and persistent difficulty with initiating sleep, which were associated with greater estimated age-related brain atrophy as measured by MRI.”
Sleep plays a role in clearing out beta-amyloid, the protein that accumulates in the brains of people who develop Alzheimer’s disease, Cheng noted.
Sleep plays a role in clearing out beta-amyloid, the protein that accumulates in the brains of people who develop Alzheimer’s disease. (REUTERS/Denis Balibouse)
When someone gets poor sleep, that clearance ability is reduced.
“Being readily identifiable, the onset of these symptoms may represent a key timepoint during which intervention could mitigate the development of disorders such as Alzheimer’s disease later in life,” Cheng added.
Potential limitations
The study did have some limitations, including the fact that it relied on people reporting their own sleep habits, which may not always be accurate, according to Cavaillès.
“Also, because this was an observational study, we can’t say for certain that poor sleep directly causes brain aging — only that there’s a strong connection between the two,” he added.
“This study provides further support for the integral relationship between sleep and brain health.”
Cheng agreed that causation cannot be determined from the study, and also noted that it did not investigate whether brain atrophy had an impact on cognition.
Despite these limitations, she said, “There are plausible roles that poor sleep may play in brain health.”
Improving sleep quality
Based on the findings, people can improve their quality of rest by adopting several good sleep hygiene practices, Cavaillès said.
CLICK HERE TO GET THE FOX NEWS APP
“They can start by maintaining a consistent sleep schedule, going to bed and waking up at the same time every day,” he said.

Regular exercise can help improve sleep quality, experts agree. (iStock)
“Creating an ideal sleep environment — keeping the bedroom dark, quiet and at a cool temperature — also helps.”
Regular exercise and exposure to natural sunlight can also improve sleep quality.
CLICK HERE TO SIGN UP FOR OUR HEALTH NEWSLETTER
Cavaillès also suggests avoiding screens and blue light, as well as stimulants like caffeine and alcohol.
“Incorporating relaxation techniques before bed, such as deep breathing or meditation, can also help prepare the body for sleep,” the researcher added.

Healthy sleep is essential for a healthy brain, experts agree. “If someone is facing persistent problems with sleep quality or insomnia symptoms, they should undergo further evaluation,” a doctor advised. (iStock)
Cheng echoed that healthy sleep is essential for a healthy brain, hence the importance of maintaining good sleep habits.
“If someone is facing persistent problems with sleep quality or insomnia symptoms, they should undergo further evaluation,” she said.
For more Health articles, visit www.foxnews.com/health
“This may be indicative of an underlying disorder, such as obstructive sleep apnea, and intervention may improve both quality of life and overall health.”
The study was funded by the National Institute on Aging.

